Promoting Well-being through Counselling
Our diverse programs designed for comprehensive healthcare and community empowerment. From our STI and Staff Clinic and Mobile Clinic delivering essential medical services to our COE Clinic's focus on HIV prevention and treatment, we ensure quality healthcare reaches all. With our rigorous Laboratory standards and supportive Counselling team, we prioritize research integrity and psycho-social well-being.
Comprehensive Healthcare at RHSP STI and Staff Clinic
The Rakai Health Sciences Program (RHSP) extends its commitment to healthcare beyond the community through its STI and Staff Clinic. This facility caters to the outpatient medical needs of RHSP staff and their children under 5 years, ensuring convenient access to quality healthcare without disrupting their work responsibilities. While the clinic offers primary care services, individuals with complex illnesses requiring specialized treatment are referred to higher-level facilities for comprehensive management.
Services Offered
Outpatient Medical Care
RHSP staff and their young children benefit from the convenience of on-site medical care, which not only ensures timely access to treatment but also reduces the need for extended absences from work or school. This service helps to promote a healthy work-life balance for employees and supports the overall well-being of the RHSP community.
Referral Services
In situations where the expertise and resources available at the current healthcare facility may not be sufficient to address the complexity of a patient's condition, it is crucial to promptly refer the case to a higher-level healthcare facility. This proactive approach to referrals helps ensure that patients receive the level of care that is most suitable for their specific needs, leading to better health outcomes and overall patient satisfaction.
STI Screening & Management
Providing free STI screening and management services to RCCS participants is crucial for promoting sexual health and preventing STI spread within the community. This initiative encourages individuals to prioritize their sexual health, seek treatment when needed, and contributes to reducing STI prevalence. Through regular screenings and effective management, the RCCS is proactively safeguarding participant health and creating a healthier, more informed community.
The RHSP STI and Staff Clinic serve as a prime example of the organisation's unwavering dedication to providing comprehensive healthcare services to its staff members and the wider community. Through the provision of on-site medical care and a range of specialised services, including STI screening and management, RHSP continues to make a significant impact in enhancing healthcare access and promoting public health initiatives in the Rakai region. The presence of these clinics not only ensures that employees receive timely and quality healthcare services but also extends these benefits to the local community, thereby contributing to the overall well-being and health outcomes of the region.

Enhancing Healthcare Access with the RHSP Mobile Clinic
As part of its commitment to community health and well-being, the Rakai Health Sciences Program (RHSP) operates a Mobile Clinic to deliver essential medical services alongside the Rakai Community Cohort Study (RCCS) activities. This initiative aims to bridge healthcare gaps by providing diagnosis and symptomatic management of outpatient illnesses directly within the communities.
Key Services
1. General Medical Care: The RHSP Mobile Clinic offers comprehensive medical care, addressing a wide range of outpatient illnesses. From common ailments to more complex conditions, the clinic provides timely diagnosis and management to community members.
2. Referral Services: In cases where specialised care is necessary, the clinic facilitates referrals to higher-level healthcare facilities. This ensures that individuals receive appropriate treatment and follow-up care, optimising health outcomes.
Impact on RCCS Participation
The provision of medical services through the Mobile Clinic plays a crucial role in motivating community members to engage in RCCS activities. By offering accessible healthcare within the community, participants are more likely to actively participate in research activities, contributing to the success and effectiveness of the RCCS.
The RHSP Mobile Clinic exemplifies the organisation's commitment to promoting community health and facilitating research activities. By bringing essential medical services directly to the doorstep of community members, the clinic not only improves healthcare access but also strengthens community engagement in health research initiatives such as the RCCS.

Empowering Communities with HIV Services: The RHSP Centre of Excellence (COE) Clinic
The RHSP Centre of Excellence (COE) Clinic stands as a beacon of hope for HIV prevention, care, and treatment services in Kalisizo and its surrounding areas. With a comprehensive range of services tailored to meet the diverse needs of its clients, the COE Clinic plays a pivotal role in promoting health and well-being within the community.
Key Services Offered
1. HIV Testing Services: The clinic provides confidential HIV testing services, ensuring early detection and timely initiation of treatment.
2. Antiretroviral Therapy (ART) Services: Both paediatric and adult ART services are available, catering to the specific needs of different age groups.
3. Cervical Cancer Screening: Regular cervical cancer screening services are offered to enhance women's health and well-being.
4. Early Infant Diagnosis and Treatment: The clinic focuses on eliminating mother-to-child transmission of HIV through early infant diagnosis and treatment interventions.
5. Tuberculosis (TB) Screening and Treatment: Screening and treatment services for TB are provided to address co-infections and improve overall health outcomes.
6. TB Preventive Therapy (TPT): The clinic offers TB preventive therapy to individuals at risk of developing TB, contributing to disease prevention efforts.
7. Pre-exposure Prophylaxis (PrEP) and Post-exposure Prophylaxis (PEP): PrEP and PEP services are available to individuals at risk of HIV infection, offering effective preventive measures.
8. Family Planning Services: Family planning services are integrated into the clinic's offerings, promoting reproductive health and choice.
9. Viral Load Testing: Regular viral load testing is conducted to monitor treatment efficacy and ensure optimal outcomes for clients.
Patient-Centered Care
To enhance patient retention and engagement, the COE Clinic adopts differentiated service delivery models. These models include both clinic-based care and community outreach programs, ensuring accessibility and continuity of care for clients.
Impact and Achievements
By December 2023, the COE Clinic had a remarkable impact, serving 2,647 active clients on antiretroviral therapy. Impressively, 98% of these patients achieved viral suppression, a testament to the clinic's commitment to quality care and treatment outcomes.
Support and Collaboration
The COE Clinic's activities are made possible through support from a sub-grant under the IDI PEPFAR grant, enabling the continuation and expansion of vital HIV services within the community.
The RHSP Centre of Excellence (COE) Clinic stands as a cornerstone in the fight against HIV/AIDS, providing essential services and support to individuals and families affected by the virus. Through its holistic approach and collaborative efforts, the clinic continues to make significant strides towards achieving HIV elimination goals and promoting community health and well-being.
The RHSP Counselling Section stands as a pillar of support within the Rakai Health Sciences Program's (RHSP) research and programs directorate. With a mandate to provide ongoing psycho-social support counselling, the section plays a vital role in safeguarding the well-being of research participants, patients, staff, and other community members within RHSP-supported communities.
Core Responsibilities
Psycho-social Support
The counselling section offers a range of psycho-social support services tailored to meet the diverse needs of individuals within the community. Whether facing challenges related to health, relationships, or personal well-being, individuals can access confidential counselling to navigate through difficult times.
Well-being Assurance
Ensuring the well-being of all stakeholders is paramount to the counselling section. By providing a safe and supportive environment, the section strives to address mental health concerns, alleviate stress, and promote resilience among community members.
Community Engagement
Through community outreach initiatives, the counselling section actively engages with community members to raise awareness about mental health, destigmatize seeking help, and encourage proactive self-care practices.
Commitment to Confidentiality
Confidentiality is upheld as a cornerstone of the counselling section's ethos. All interactions between counsellors and clients are treated with the utmost discretion and respect for privacy, fostering an environment of trust and openness.
The RHSP Counselling Section exemplifies the organization's dedication to holistic health and well-being. By offering compassionate support and guidance, the section plays a vital role in nurturing resilient communities and fostering a culture of care and support within RHSP-supported areas.
Empowering Our Communities: Health Education and Community Mobilisation (HECM)
The Health Education and Community Mobilisation (HECM) section serves as the vital link between the Rakai Health Sciences Program (RHSP) and the communities where research and program activities are carried out. With a primary focus on community engagement, the HECM section plays a pivotal role in fostering awareness, participation, and collaboration within these communities.
Core Functions
- Community Awareness: The HECM section is dedicated to raising awareness about RHSP research initiatives, as well as the various services and programs offered. Through targeted educational campaigns and outreach efforts, community members are informed about the importance of research participation and encouraged to actively engage in RHSP activities.
- Compliance and Participation: By fostering a sense of ownership and involvement, the HECM section aims to increase community compliance and participation in RHSP endeavors. Through community mobilization efforts, individuals are encouraged to take an active role in their own health and well-being.

Friendly Environment Creation: Creating a welcoming and supportive environment is paramount to the success of RHSP activities. The HECM section works to cultivate positive relationships and trust within communities, ensuring that research and program activities are conducted in a manner that is respectful and responsive to community needs.

Additional Activities
- Dissemination of Research Findings: The HECM section ensures that research findings are effectively communicated to the communities involved, fostering transparency and accountability.
- Preparation for Services: Communities are prepared and informed about the various services offered by RHSP, facilitating access and utilisation.
- Community Advisory Board (CAB) Collaboration: Working closely with the Community Advisory Board (CAB), the HECM section facilitates dialogue and feedback between research communities and RHSP, ensuring that research activities are conducted in a manner that is ethical, respectful, and beneficial to all parties involved.
The HECM section serves as a cornerstone of community engagement within RHSP-supported areas. By fostering awareness, participation, and collaboration, the section contributes to the success and impact of RHSP research and program activities, ultimately improving health outcomes and well-being within the community.
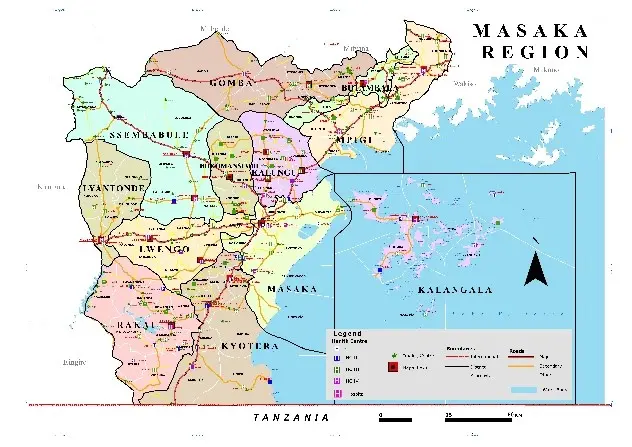
The Masaka HIV Regional mechanism (2017-2023)
The Health Education and Community Mobilization (HECM) section serves as the vital link between the Rakai Health Sciences Program (RHSP) and the communities where research and program activities are carried out. With a primary focus on community engagement, the HECM section plays a pivotal role in fostering awareness, participation, and collaboration within these communities.
In
April 2017, Rakai Health Sciences Program (RHSP) received the PEPFAR award for
a Cooperative Agreement (CoAG) with the Centers for Disease Control and
Prevention (CDC) to accelerate Epidemic Control in Masaka Region (Accelerating Epidemic Control in Masaka
Region in the Republic of Uganda
under President`s Emergency
Plan for AIDS Relief,
Award No. 5NU2GGH002009). The goal was to support comprehensive HIV/AIDS prevention, care, and treatment
services to persons in 12 districts in Masaka Region. These included the
districts of Lwengo, Bukomansimbi, Lyantonde, Kalungu, Masaka, Mpigi, Gomba,
Sembabule, Butambala, Kalangala, Rakai and Kyotera districts.
The project involved capacity building of the district leadership to plan, coordinate, supervise, monitor, evaluate and fully own the implementation of HIV programs in addition to strengthening of health facility and community level (District Led Programming (DLP).
Project implementation was geared towards achieving an AIDS free generation by targeting populations at the greatest risk of HIV and in urgent need of services in line with the revised UNAIDS 95-95-95 targets and the PEPFAR priorities.
The project objectives were:
• Use targeted HIV testing service (HTS) models to men, key populations (KP) and priority populations (PP) to improve identification of PLHIV in community and health facilities in scale-up districts.
• Provide combination prevention interventions to KP/PP scale-up districts.
• Provide linkage to high-impact prevention, ART, and other community services.
• Provide ART services to all eligible PLHIV as outlined in the latest national HIV treatment guidelines:
• Improve coverage and quality of integrated eMTCT, EID, better track newly enrolled maternal and infant outcomes:
• Work with DHTs and Health Facilities to reduce TB burden in PLHIV and HIV in TB clients:
• Support the national commodity supply chain systems:
• Strengthen lab quality management systems for CQI in viral load, laboratory sample transportation/results transmission system, and other HIV related testing.
Strengthened governance and oversight functions at district level for joint planning, coordination, support supervision, and performance monitoring for sustained epidemic control.
HIV Prevention, Care and Treatment Services (2004 - 2017)
From June 2004 to September 2017, HIV services were provided in the districts on Rakai, Kyotera and Lyantonde. The services were funded by the President’s Emergency Plan for AIDS Relief (PEPFAR) through a subgrant from the Makerere School of Public Health, Cooperative Agreement (CoAG) with the US Centers for Disease Control and Prevention (CDC) to develop human resource capacity for management of HIV/AIDS and other health programs in Uganda and deliver comprehensive community based HIV/AIDS prevention, care and treatment services to persons at risk of getting HIV and HIV infected persons and their family members in Rakai and surrounding districts. RHSP supported the provision of comprehensive HIV/AIDS prevention, care and treatment to HIV positive clients using the District-led HIV programming approach. RHSP also supported provision of Voluntary Medical Male Circumcision, Pre-exposure prophylaxis and DREAMS (Determined, Resilient, Empowered, AIDS-free Mentored and Safe).
The overall goal of this project was to scale up of comprehensive HIV prevention, HIV/ Tuberculosis (TB) care, HIV care and treatment services in Rakai district through a district-led approach.
The project implementation strategy focused on provision of HIV prevention, care and treatment to children and adults through community-based clinics located in Rakai and Lyantonde districts. In an effort to take services closer to the patients, services were provided initially through seventeen (17) HIV clinics then through 35 government health facilities, including, hospitals, health center IV, III and II.
Services Offered

1. Abstinence and be faithful (AB) and other prevention activities:
Activities focused on targeted health education in small groups of 25 people each, and condom distribution, sensitization meetings for community and opinion leaders, village meetings, film and drama show. Education (HE) sessions addressed a wide range of messages including HIV prevention (abstinence, being faithful to one partner and condom use), the need to receive HIV testing, timely enrollment into HIV care upon receipt of a positive HIV result, adherence to treatment (ART and prophylaxis), and availability of and access to medically performed male circumcision (MMC) for prevention of HIV. We reached most at risk populations like fishing communities and female sex workers, youth in and out of schools, married couples, and discordant couples.
2. Palliative Care: Basic Health Care and Support: A wide range of
basic HIV care services were provided including; screening for sexually transmitted infections like syphilis, provision of health education especially positive prevention messages at the HIV clinics, distribution the basic care package (containing mosquito bed nets for prevention of malaria, a clean water vessel, filter cloth and hypochlorite solution for water treatment, for prevention of diarrheal diseases), condom distribution, treatment and prophylaxis of opportunistic infections like Tuberculosis, cryptococcal meningitis, pneumocystis jiroveci pneumonia ( with supply of daily cotrimoxazole).We promoted integration of nutritional services in HIV care by empowering patients to use the locally available foods to prevent malnutrition. We also trained health providers to identify patients in need of referral for nutritional management was also built. All HIV positive patients received laboratory support for monitoring of CD4 count progression and for diagnosis of opportunistic infections.
3. Antiretroviral therapy (ART): We provided ART to both children and adults. Adherence to ART was tracked through home visits, initially by nurses and later by trained peer educators. Patients initiated on ART were visited monthly at home, to check and support adherence to treatment. Adherence counseling was given prior to ART initiation, during home visits and through all other interactions with the patients. As a result, over 95% of the patients achieved 100% adherence to treatment. To ensure quality care, patients initiated on ART were monitored clinically, immunologically (using CD4 count evaluation) and virologically, either six monthly or annually. Patients failing on ART were identified through the viral load database system and discussed /evaluated for second line therapy. To facilitate durability of second line regimens, surprise home visits were conducted at home to verify adherence before change to second line treatment.

The peer support program entails support groups attached to all clinics offered adherence support to fellow patients on ART. They also helped identify clients with social and other problems which might impact treatment outcomes. For patients or caretakers of children with difficulty understanding the ART dosages, the peer supports assisted with Directly Observed Therapy until the patients fully understood drug dosing.
4. Laboratory infrastructure: The RHSP laboratory supported all HIV testing and monitoring for biological samples collected from the HIV clinics and HIV counseling and testing centers within Rakai and Lyantonde districts. The only exception was the qualitative PCR for infant diagnosis, which is provided MOH central public health laboratory. The laboratory provided a range of tests including HIV testing (rapid testing), serology like syphilis, Cryptococcus (serum CRAG) testing, microbiology testing like TB diagnosis, molecular e.g. viral load testing, CD4 count testing, and chemistry tests. The laboratory quality control and assurance staff provided support supervision and quality assurance, ensuring accurate performance. We supported district health center laboratory diagnosis of opportunistic infections through training of the lab staff, provision of supplies and microscopes.
5. TB/HIV care was provided to all clients enrolled in the HIV clinics. All clients who came into contact with the HIV clinic system were screened for TB through clinical evaluation. ART clients were screened using the Intensified Case Finding Form (ICF) while pre-ART clients were screened at the time of the clinical assessment. If indicated (i.e. Signs or symptoms of tuberculosis present), such patients were further investigated using sputum examination (Ziehl-Neilsen (ZN) smear. All TB positive patients received anti-TB treatment. We supported integration of TB treatment into the existing government health units, and trained laboratory staff to diagnose TB provision of laboratory reagents, to address stock outs. All care providers received training in comprehensive HIV care.
6. Prevention of Mother to child transmission of HIV (PMTCT): We provided PMTCT services to 725 pregnant women and their babies exposed to HIV. PMTCT activities included provision of antiretroviral prophylaxis for mothers and their babies, infant feeding education to encourage safe feeding options as well as reproductive health (family planning) services for the mothers. All services were provided in accordance with the Ministry of Health guidelines, and practices changed as per MOH changes. All babies born to HIV positive mothers were tested for HIV using HIV-1 DNA PCR at 4-6 weeks with the aim of early HIV diagnosis among the exposed infants. Exposed babies who initially test negative were followed up for repeat testing until HIV infection is definitely excluded. Babies who tested HIV positive were initiated on ART. Mothers of babies exposed to HIV will were educated on how to feed their babies, including ideal breastfeeding practices, weaning feeds and food preparation.
7. HIV
counseling and testing (HCT): We provided HCT
through community outreaches and at the HIV clinics and for men seeking medical
male circumcision services. We greatly encouraged couple and family HCT.
Caretakers of children were encouraged to bring the children under their care
for HIV testing. The HIV negative partners in discordant relationships were
followed up for quarterly re-testing and referred to discordant couple clubs
for continued support and HIV prevention initiatives. Unlike the previous years where we used ELISA
for HIV testing, in the latter period of this reporting period, we adopted
Uganda Ministry of Health HIV testing guidelines, using rapid HIV testing. This
highly promoted immediate HIV result receipt.

We also targeted male partners of the eligible AGYWs, to provide ART for HIV-positive men 15-49 years and VMMC for HIV-negative uncircumcised men 15-49 years.
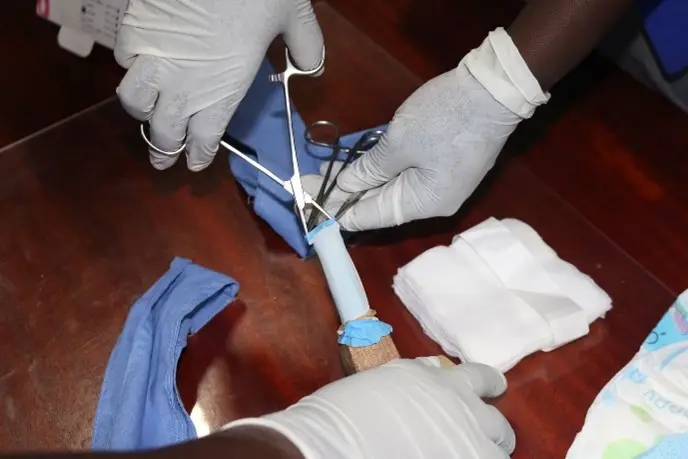
8. Voluntary
Medical Male Circumcision (VMMC): These services were
conducted at both facility and community outreaches/ MC satellite clinics and
surgical camps. Activities involved provision of surgery and medical treatment
to male clients, following-up of circumcised clients to assess wound healing
progress, training of Circumcision service providers including regional MC
skills training, Medical Male Circumcision (MMC) training of trainers (TOT)
course, support supervision of MMC providers, offering VCT/HCT to MC clients,).
Surgical camps were conducted in collaboration with the Uganda ministry of
health (MOH) staff, Military Barracks, Police barracks, Prisons and other local
stake holders.
8. DREAMS: Since October 2016, we started delivery of the DREAMS (Determined Resilient Empowered AIDS-free Mentored Safe women) program to adolescent girls and young women at risk of acquiring HIV.
The DREAMS intervention targeted;
1. Pregnant women 15-24 years
2. Married women 15-19 years
3. Women 15-24 years who gave birth by 15 years
4. Women 15-24 years in transactional sex
5. In-school girls 15-19 years
6.HIV-negative uncircumcised men 15+ years and
7. HIV-positive men 15+ not receiving HIV care.

The core package of activities for the adolescent girls and young women (AGYWs) included:

1. Combined social-economic strengthening
2. Expanded contraceptive mix
3. Post-violence care
4. Parenting and caregiver programs
5. HIV testing and counseling
6. Condom promotion and provision
7. Community mobilization and norms change
8. Cash transfers.
We also targeted male partners of the eligible AGYWs, to provide ART for HIV-positive men 15-49 years and VMMC for HIV-negative uncircumcised men 15-49 years.
10. Infrastructure improvement: The project also tremendously supported infrastructure improvement to ensure continuity of HIV prevention, care and treatment services. This included renovation of ART clinic rooms, maternity wards, laboratories, theatres, patient waiting sheds, and latrines. We also supported installation of solar power to support maternity services and electronic data entry.
By September 30th, 2017, RHSP had provided ART to over 24,000 HIV positive adults and children, provided medical male circumcision to over 140,000 men and provided the DREAMS program to 50,196 AGYW.
Join us in our mission to advance health research and improve public health outcomes globally.
Collaborate for Health, Innovate for Impact.


