Long-term Impact of Universal Treatment and Dolutegravir on Population HIV Virologic and incidence outcomes in Africa (Long-term view Study)
The Longview Study, nested within the Rakai Community Cohort Study in Uganda, is a population-level, prospective assessment of viral load suppression, HIV drug resistance, and incidence before and after COVID-19, involving ~20,000 participants across 40 communities with high HIV prevalence and drug resistance, spanning multiple surveys from 2013 to 2025.
The Rakai Community Cohort Study (RCCS) - Understanding its Significance
The Rakai Community Cohort Study (RCCS), initiated in 1994, stands as a pioneering effort in HIV research and population-based cohort studies. RCCS is an ongoing endeavor, enrolling consenting adult residents aged at least 15 years old from 30 continuously surveyed communities. Initially focused on individuals up to the age of 49, RCCS expanded its scope in 2021 to include older participants, broadening its reach and impact.
Data Collection and Methodology
RCCS collects a wealth of data through detailed interviews covering socio-demographic, behavioral, sexual network, mobility, and health-related aspects. Additionally, participants undergo non-communicable diseases risk assessments and provide blood samples for testing, facilitating comprehensive research endeavors.
Conducting Household Census
Prior to each survey visit, RCCS conducts household censuses, capturing vital information such as household composition, births, deaths, dwelling characteristics, and mobility data. This meticulous process ensures robust data collection and analysis.


Key Features and Contributions
RCCS serves as a cornerstone for various research initiatives, hosting over 40 nested studies and sub-studies over its 35-year history. Its extensive database and longitudinal design make it an invaluable resource for understanding HIV epidemiology, health service utilization, and behavioral dynamics.
Health Services Evaluation and Clinical Trials
RCCS plays a pivotal role in evaluating health service delivery programs, including HIV care, voluntary medical male circumcision, and other health promotion initiatives. Moreover, it serves as a platform for conducting clinical trials, enabling researchers to develop and test hypotheses effectively.
Key Statistics and Findings
Response Rates
With approximately 18,000 participants, RCCS boasts a commendable response rate of about 78% among age-eligible individuals. Moreover, compliance with specimen provision for testing exceeds 90%, highlighting the community's active involvement in research efforts.
HIV Incidence
The study's longitudinal data sheds light on HIV incidence rates, spanning from around 0.9/100 person years in rural settings to 3.5-4/100 person years in fishing villages, emphasizing the localized dynamics of HIV transmission.
HIV Prevalence
RCCS findings reveal varying HIV prevalence rates, ranging from approximately 14% in rural trading villages to 42% in high-risk fishing communities on Lake Victoria, underscoring the diverse epidemiological landscape.
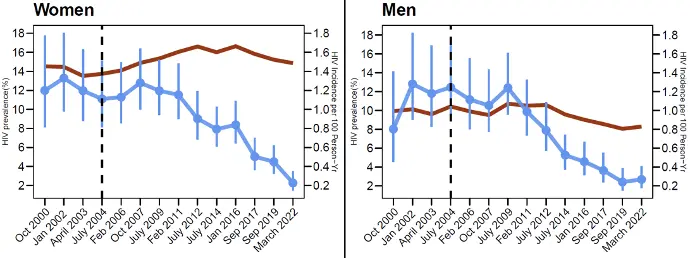
See Graph
The Rakai Community Cohort Study stands as a beacon of scientific inquiry and community engagement in the realm of HIV research. Through its comprehensive approach and longitudinal design, RCCS continues to unravel critical insights into the epidemiology, prevention, and management of HIV/AIDST
The Combination HIV Prevention Impact Evaluation (CHPIE) nest in the RCCS
To assess the effects of Combination HIV Prevention Impact Evaluation (CHPIE) coverage on population-level HIV incidence in Rakai Community Cohort Study (RCCS) communities. This is achieved by utilizing longitudinal cohort data from the general and key affected populations, and prospectively assess the impact of CHP coverage on HIV incidence.
To assess the numbers of residents throughout the
evaluation districts who accept CHP services including test and treat, PrEP,
DREAMS, and to track the numbers of new and continuing HIV care/ART clients by
age, gender and service, in order to evaluate the prevention and treatment
cascade in the study districts (i.e., the proportions of the population
receiving HCT, and proportions of HIV+ linked to care, initiating ART, adherent
to ART and virally suppressed).
Some of the earlier findings from this evaluation
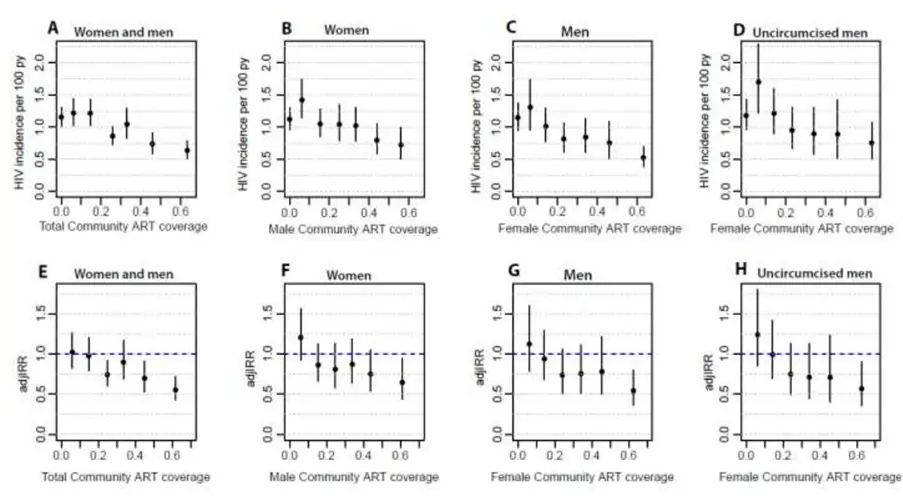
HIV incidence and individual HIV risk as a function of community ART coverage in the total population, women, men and uncircumcised men. Data are plotted at the median coverage-level within each community-level ART coverage category. (NEJM Grabowski et al 2017)
RCCS Dashboard
The Rakai Community Cohort Study (RCCS) dashboard enables researchers to explore long-term HIV incidence and prevalence trends in agrarian, trading, and fishing communities located in Rakai region of south-central, Uganda from 1994 to 2016. In addition, researchers can explore the impact of the combination HIV prevention strategy including HIV counseling and testing, voluntary medical male circumcision, antiretroviral therapy for participants living with HIV, and behavioral change on trends in HIV infection.
Understanding the Sex Partner Study: Unravelling Genital Microbiome Dynamics
Introduction to the Study
The Sex Partner Study, also referred to as the 'Assessing dynamics of heterosexual transmission of genital bacteria and coital impact on microbiome composition/stability in the female and male genital tracts in South-central Uganda,' marks a groundbreaking initiative among African couples. It delves into the intricacies of penile-vaginal sex's effects on genital microbiome composition and stability, examining the roles of various factors including biotic, abiotic, immune factors, and standard bacterial vaginosis (BV) treatment on the microbiota of both female and male genital tracts.

Primary Objectives
The primary objective of this study is to shed light on the sexual transmission of genital bacteria and elucidate the determinants influencing the penile microbiome post-sexual activity. By evaluating factors such as pH, oxygen levels, moisture, metabolites, and host and partner triad strains, researchers aim to gain insights that could lead to the development of novel antimicrobial treatments and enhance strategies like medical male circumcision to effectively mitigate HIV risk factors.
Key Focus Areas
The Sex Partner Study aims to:
- Investigate the source, diversity, and carriage characteristics of genital bacteria.
- Define the factors affecting penile microbiome outcomes after sexual activity and antimicrobial treatment.
- Enhance understanding of HIV risk factors and their epidemiology and biology.
Study Design and Participants
This prospective study plans to enrol up to 164 heterosexual couples, comprising HIV-negative adults aged 18-45, who are existing sexual partners. Partnership must have engaged in

in unprotected penile-vaginal sex for at least a month, not used oral antibiotics in the past three months, and have no history of immunosuppressive diseases or current STI symptoms.
Methodology
Study activities involve the collection of pre- and post-coital samples to analyze the impact of penile-vaginal sex and associated factors on the temporal composition and stability of the genital microbiome among heterosexual couples.
The Sex Partner Study represents a significant step forward in understanding the dynamics of genital microbiota and its implications for HIV transmission. By exploring the intricate interplay of various factors, this study holds promise for developing innovative approaches to reduce HIV risk factors and enhance overall sexual health outcomes.
Empowering Our Communities: Health Education and Community Mobilization (HECM)
The Health Education and Community Mobilization (HECM) section serves as the vital link between the Rakai Health Sciences Program (RHSP) and the communities where research and program activities are carried out. With a primary focus on community engagement, the HECM section plays a pivotal role in fostering awareness, participation, and collaboration within these communities.
The health education and community mobilization (HECM) section is the community engagement arm that links the Rakai Health Sciences Program to the communities where organization research and program activities are executed. The core function of HECM is to create community awareness about RHSP research and services/programs, increase compliance and community participation and create a friendly environment for research and program activities to be implemented. Other activities include:
Core Functions
- Community Awareness: The HECM section is dedicated to raising awareness about RHSP research initiatives, as well as the various services and programs offered. Through targeted educational campaigns and outreach efforts, community members are informed about the importance of research participation and encouraged to actively engage in RHSP activities.


- Compliance and Participation: By fostering a sense of ownership and involvement, the HECM section aims to increase community compliance and participation in RHSP endeavors. Through community mobilization efforts, individuals are encouraged to take an active role in their own health and well-being.
- Friendly Environment Creation: Creating a welcoming and supportive environment is paramount to the success of RHSP activities. The HECM section works to cultivate positive
relationships and trust within communities, ensuring that research and program activities are conducted in a manner that is respectful and responsive to community needs.
Additional Activities
- Dissemination of Research Findings: The HECM section ensures that research findings are effectively communicated to the communities involved, fostering transparency and accountability.
- Preparation for Services: Communities are prepared and informed about the various services offered by RHSP, facilitating access and utilization.
- Community Advisory Board (CAB) Collaboration: Working closely with the Community Advisory Board (CAB), the HECM section facilitates dialogue and feedback between research communities and RHSP, ensuring that research activities are conducted in a manner that is ethical, respectful, and beneficial to all parties involved.
The HECM section serves as a cornerstone of community engagement within RHSP-supported areas. By fostering awareness, participation, and collaboration, the section contributes to the success and impact of RHSP research and program activities, ultimately improving health outcomes and well-being within the community.
Unveiling the Enigma of Hard-to-Reach Individuals: The Hard-to-Reach Research Study 2021-2024
Defining Hard-to-Reach (HTR) Persons
In the realm of the Rakai Community Cohort Study (RCCS), Hard-to-Reach (HTR) individuals pose a unique challenge. These are individuals who have eluded detection by the regular RCCS outreach efforts on at least two separate occasions. The repeated absence of these individuals raises concerns about potential differences between them and the surveyed population, necessitating a closer examination of conclusions drawn from the sampled data.
Objectives of the Hard-to-Research Study
The Hard-to-Research Study, spanning the years 2021-2024, embarks on a journey to unlock the mysteries surrounding HTR individuals, with the following aims:
A Section Subtitle
Write one or two paragraphs describing your product or services. To be successful your content needs to be useful to your readers.
Start with the customer – find out what they want and give it to them.


Aim 1
To ascertain the coverage of combination HIV prevention (CHP) strategies and determine HIV incidence rates among hard-to-reach individuals, leveraging enhanced surveillance techniques.
Aim 2
Delineate sources of ongoing HIV infections through meticulous partner tracing of newly HIV-infected participants and matched HIV-negative controls. Involves using viral phylogenetic and sexual network analyses to unravel the dynamics of HIV transmission.
Aim 3
To assess the efficacy of state-of-the-art CHP interventions in engaging hard-to-reach populations and ultimately reducing population-level HIV incidence to levels conducive for HIV elimination by 2030.
Methodology and Research Approach
The core of this study revolves around characterizing the sources of incident HIV infections through a multi-faceted approach:
- Partner Tracing: Identifying sexual partners of RCCS participants recently diagnosed with HIV (termed 'incident cases') and matching them with HIV-negative controls.
- Enrolment of Partners: Enrolling identified partners in the RCCS, irrespective of their residence or community boundaries.
- Next-Generation Sequencing: Obtaining HIV sequencing data from seroconverters and HIV-positive partners to validate self-reported partner networks, ascertain probable infecting partners, and delineate potential transmission dynamics.
The Hard-to-Research Study represents a pioneering effort to shed light on the enigmatic realm of hard-to-reach individuals in HIV research. By employing innovative methodologies and cutting-edge techniques, this study aims to not only deepen our understanding of HIV transmission dynamics but also pave the way for more effective prevention strategies, ultimately inching closer to the goal of HIV elimination by 2030.
Epidemiology and Impact of the HIV, NCD, and Urbanization Syndemic in Africa.
Objectives
Aim 1: Characterize HIV-related and -unrelated risk factors for cardiopulmonary non-communicable diseases (CP-NCDs) in a novel Rural-to-Urban (R2U) African cohort.
Aim 2: Characterize the impact of air pollution and moderating effects of HIV on cardiopulmonary clinical outcomes among R2U migrants.
Aim 3: Assess HIV and CP-NCDs health services utilization patterns among R2U migrants [and design an integrated HIV/CP-NCD intervention.
Methodology
The study is nested in RCCS. Rural to urban migrants (Masaka city and Kampala metropolitan) are the indexes. Each index is matched on sex, age, HIV status and community with one rural to rural migrant and two non-migrant participants.
Activities
1. Spirometry: done on all eligible participants using NDD software.
2. Echocardiography: 2,847 participants had echocardiogram done on them during round one of the study.
3. Air-quality monitoring
a) Personal exposure air quality monitoring: Sets of carbon monoxide monitors and ECM monitors are worn and placed in the cooking area for 48hours to capture carbon monoxide concentration and PM_2.5 data.
b) Ambient
Air Quality monitoring: we use purple air
devices that were placed in various places (17 in RCCS communities, placed at
Health facilities, 4 in Masaka and 4 in Kampala metropolitan). One was
collocated with BAM at Makerere University weather station and 3 were
collocated with Airqo devices. One purple air device was

collocated with the E-sampler to RHSP headquarters for data validation.

4. Ambulatory Blood pressure Monitoring: 24our ABPM is done on a selected group of participants in the VICINITY study.
5. Daily
movement mapping: used GPS logger to map out the
routes and locations where participants passed or spent their time in 24hours.
SBS Department Overview:
The Social and Behavioral Sciences department (SBS) at Rakai Health Sciences Program (RHSP) focuses on gathering and analyzing qualitative research data (non-numerical data) to understand human behavior, attitudes, beliefs, and motivations. Overall, it enriches the understanding of human behavior, informing strategic decisions, and advancing knowledge in the field of HIV through rigorous inquiry.
Aims of the department:
Exploring human experiences & social contexts beyond quantitative methods. We aim to gather and explore contexts using the multiple techniques we use.
Using techniques like interviews, focus groups, observations, and content analysis to generate in-depth, nuanced insights for decision-making and theory-building.
Understanding the perspectives, opinions, and interpretations of individuals or groups, often involving a smaller sample size but with a deeper level of engagement.
Contributing to theory development by generating hypotheses, finding patterns, and exploring new ideas to deepen existing knowledge.
Relevance of the SBS department within RHSP.
- Design, execute, and analyze qualitative research data that address specific research questions or objectives.
- Collaborate with in country and outside research partners, quantitative researchers, interdisciplinary teams, and stakeholders to integrate qualitative insights into broader research initiatives and interdisciplinary projects.
- Offer expertise in qualitative research methods, including study design, data collection, analysis techniques, and interpretation of findings, to support the research needs of the organization, universities, and collaborators.
- Provide actionable insights and recommendations based on qualitative research findings to inform strategic decisions, program development, policy formulation, and organizational practices.
- Communicate research findings through reports, presentations, publications, and other dissemination channels to share knowledge with internal and external stakeholders, contribute to discussions, and promote evidence-based practices.
Past and Current Areas/Projects (Selected)
A. Assessing dynamics of heterosexual transmission of genital bacteria and coital impact on microbiome composition/stability in the female and male genital tracts in South-central Uganda (Sex Partner study)
Objective:
Primary: To elucidate the sexual transmission of genital bacteria and the determinants of the penile microbiome after sex.
Secondary: To qualitatively assess study participant perspectives and overall experience with study procedures.

B. PANGEA
Qualitative research to understand sexual relationships where phylogenetic links are missing (The Missing Links)
Objective:
To better understand the sexual relationships of female RCCS participants who are part of the identified incomplete phylogenetic networks that reflect likely HIV transmission.
C. WHO
Cognitive Testing of a Survey Instrument to Assess Sexual Practices, Behaviors, and Health Related Outcomes:
Objective: To Refine a Standard Instument in English and other Language Versions by testing it in a variety of Demographic Cross Sections of the General Populations, e.g older persons, persons in rural areas worldwide.


D. PANGEA
Fishing and Inland Communities – Understanding Transmission Linkages and Networks.
Objective:
To gain a deeper understanding into underlying factors that drive preferential migration of people living with HIV to high prevalence Lake Victoria fishing communities, and the reasons for lower ART use among these migrating populations.
e. Baseline, Midterm and End of Project Evaluation Protocol for Masaka Regional mechanism (Program Evaluation - Mid-Term, 2021 and End Term, 2022)
Objective:
- To collect data that will inform improvement of program implementation so that services are provided more effectively and efficiently in the region and best practices shared with other IPs in the country.
- To also inform RHSP, CDC and other stakeholders about program challenges, performance gaps, progress towards achievement of set targets and program outcomes (effectiveness) in a timely manner so that implementation strategies can be maintained, scaled up or modified where necessary.
f. Impact of COVID-19 Lockdown on HIV and Reproductive, Maternal, Neonatal, and Child Health (RMNCH) Services in Masaka region, Uganda (2020)
Objective:
To assess the impact of the COVID-19 lockdown on utilization of RMNCH and HIV services, and assess experiences and coping mechanisms in order to make recommendations to mitigate the impact of this and similar health emergencies in the future.
g. Exploration of psychological distress and cross-cultural adaptation of a mental health measure for people living with HIV in Rakai, Uganda (2021)
Objective:
To explore mental health and psychosocial
issues among people living with HIV in rural Rakai
h. Structural and Social Transitions among Adolescents and young adults in Rakai (SSTAR): (2019 – 2020)
a. Nakubulwa Rosette: Research Officer
b. Isabirye Dauda: Research Officer
c. Ddaaki William: Supervisor
d. Nakyanjo neema: Head of Department
4. PARTNERS/COLLABORATION:
a. Columbia University
b. Johns Hopkins University
c. Medical Research Council
d. Makerere University
Background
HIV treatment in Africa has evolved dramatically in recent years with the rollout of Universal Test-and-Treat (UTT). However, despite universal test and treat rollout, HIV incidence has declined only modestly, with no African country on track to meet UNAIDS 2030 targets for epidemic control. Control efforts are challenged by substantial numbers of “hard-to-engage” HIV-positive persons who remain viremic2.
Relatedly, there have been significant increases in HIV drug resistance (HIVDR) with expanded antiretroviral therapy (ART). The growing threat of HIIV drug resistance propelled the recent roll-out of Dolutegravir (DTG), an integrase inhibitor with a high barrier to resistance.
While Universal test and treat and Dolutegravir may result in lower rates of viremia and HIVDR, there is considerable uncertainty about the magnitude and durability of their population-level impact, especially in the context of the coronavirus disease 19 (COVID-19) global pandemic, which was disrupting African HIV prevention and treatment programs supported by the United States President’s Emergency Plan for AIDS Relief (PEFAR).
To address these issues, we are conducting the Longitudinal Viral Load and Epidemiological Watch (LONGVIEW) Study, a population-level, prospective assessment of durable viral load (VL) suppression (i.e., sustained suppression over the life course), HIVDR, and incidence before and after COVID-19 emergence in southcentral Uganda.
This study is nested within the Rakai Community Cohort Study (RCCS), a prospective, population-based study of ~20,000 persons, aged 15-49 years, in 40 communities with HIV prevalence ranging from ~9 to 40% and ~20% transmitted HIVDR. We measure Viral loads and perform deep sequence viral phylogenetics on all HIV-seropositive participants over 7 surveys (n~3800 per survey) conducted between 2013 and 2025, spanning roll-out of Universal test and treat in 2017, Dolutegravir in 2019, and emergence of COVID-19 in 2020.
Objectives
- This study will quantify population and individual trends in viremia and HIV drug resistance.
- Assess the impact COVID-19 on HIV treatment seeking, utilization, and provision of care
- Measure population HIV incidence trends as well as transmission risk across the infection and care continuum
Our overarching hypothesis is that despite UTT and DTG rollout, the COVID-19 pandemic will disrupt HIV services resulting in significant declines in durable population VL suppression, increases in HIV-DR, including emergence of DTG resistance, and rising HIV incidence.
The Longview study follows individuals who are in the Rakai community cohort study who are HIV positive and virally unsuppressed according to the Ugandan national guidelines. These individuals are categorized into those who are newly diagnosed (group 2), with previous diagnosis however never been on ART (group 3) and then those who are currently or have ever been on ART but are virally unsuppressed.
These participants are followed up and an interview is conducted to establish if these clients are in care plus the facility of HIV/AIDs care and treatment and if not yet in care, then reasons for this are cited. There after clinical data about the identified participants at their respective clinics is extracted using a questionnaire identifying if they are active in care or defaulting, past & current ART regimens, CD4, current Viral loads, differentiated service delivery models and time spent on ART at the facility. We also provide counselling basing on their viral load.
International Epidemiology Databases to Evaluate AIDS (IeDEA) Consortium
Introduction
IeDEA collects observational data representing over 2.2 million people living with and at risk for HIV, contributed by clinical centers and research groups in 44 countries. IeDEA data are organized into 7 geographic regions (regional cohorts) and coordinated by centers for the Asia-Pacific, the Caribbean, Central and South America region, Central, East, Southern, and West Africa, and North America IeDEA conducts both regional and global research.
Data Use
The investigators use the IeDEA platform to share their multidisciplinary expertise and answer high-priority research questions. These include evaluating the HIV treatment cascade, co-infections like tuberculosis and hepatitis, cancers, and non-communicable diseases, including mental health and substance use disorders.

Research Team Composition
The IeDEA community is composed of investigators, study coordinators, and data teams representing multiple countries, languages, and backgrounds. Consortium members meet regularly through interest-based Working Groups to guide the collaborative research projects. Rakai Health Sciences Program (RHSP) in the East Africa region is a clinical site and research group contributing data to IeDEA. For more information, please check, IeDEA International Epidemiology Databases to Evaluate AIDS
Rakai Orphans in Communities (ROC)
Introduction
The loss of one or both parents can have devastating consequences for children, adolescents, extended families, communities, and nations. Recently, improvements in HIV treatment and prevention have led to dramatic declines in orphanhood. This appears to be the result of combination HIV prevention (CHP), particularly expanded access to highly effective antiretroviral therapy (ART) and declining HIV-related mortality among adults – adults who are often parents. The declines in HIV-related orphanhood proffer substantial benefits to children and youth, families, and their communities. Little is known about how declines in orphanhood among youth may have impacted social and economic factors that influence HIV risk as orphans move into the adolescent and young adult (AYA) years.
The specific aims for ROC study are to:
1. Define, over time, the potentially changing consequences of orphanhood including the relationship between orphanhood and HIV infection and HIV risk behaviors among youth from RCCS Rounds 6-23 (1999-2027).
2. Explore issues related to mechanism and measurement to better understand the population burden of orphanhood, heterogeneity among orphans, and the circular relationships between 1- HIV infection among adults and subsequent orphaning and 2- orphanhood and HIV risk among youth. A key issue of mechanism is the timing of orphaning (i.e., age they became an orphan) and how that affects the consequences of orphaning.
3. Through life history interviews, explore the mechanisms by which orphanhood and age at orphaning may influence HIV risk and social outcomes and begin to assess and address how programs can be tailored to meet the needs of this vulnerable population. Interviews will be conducted with youth and their adult caretakers during childhood and adolescence; each should be able to differentially report on events and circumstances of the orphaning period.
4. Estimate the economic impact of declining HIV-related orphanhood on youth, families, and communities in Rakai and in Uganda, using data from RCCS. In a cost-benefit analysis, we will examine benefits of declining orphanhood (decreased adult mortality, decreased orphanhood, increased educational status, decreased HIV infection among youth) and costs (costs for ART, MMC). Addressing HIV-related orphanhood is an important PEPFAR priority but economic impacts have received little recent scientific attention, particularly, the impact of declining orphanhood on youth risk for HIV infection.
Methods
The proposed Rakai Orphans in Communities (ROC) Study will be based in the Rakai District of southcentral Uganda- one of the districts hardest hit by HIV/AIDS. The ROC Study explores the impact, measurement, and policy issues at the intersection of orphanhood, HIV risk among AYA, adolescent social transitions, and family and social context. Impacts include HIV risk and social and economic consequences. Measurement of age at orphaning will be a critical component of this proposal. In several studies, earlier age at orphaning appears to be related to more adverse outcomes.


Expected Outcomes
We will estimate the impact of orphanhood on social and behavior risk for HIV and how that impact may change based on the age at orphaning. An under-explored component which we are to examine is the economic benefits of Combined HIV Prevention Interventions (CHP) weighed against the costs. Using the rich resources of the Rakai Community Cohort Study (RCCS), we will explore the relationship. We will address the NIH-stipulated biological variable of sex; analyses will account for sex via stratification or adjustment.
Improving understanding of Capacity to consent to biomedical HIV prevention Research among adolescents in Rakai Uganda (ICARE)
In our prior study of adolescent capacity to consent to observational research in Uganda (R01HD091003- 03S1), we used the MacArthur Competence Assessment Tool for Clinical Research (MacCAT-CR), a highly flexible tool that has accumulated the most adolescent data and described age-related capacity of adolescents to consent to lower-risk research. In this study, we will leverage The Rakai Community Cohort Study (RCCS) to test adolescent capacity to consent to biomedical research, identify differences in developmental decision-making, characterize eligibility for, beliefs about, and interest in oral and injectable pre-exposure prophylaxis (PrEP), and construct a digital toolkit for including adolescents in biomedical research. The RCCS presents a unique opportunity to compare cognitive capacity to consent for biomedical research among adolescents with and without prior research experience at three developmental stages – early (10-14 years), middle (15-17 years), and late (18-19 years) – with the cognitive capacity of their parents/guardians. Limited data are available on adolescents’ actual capacity to consent, particularly in low- and middle-income countries and low-resource, high-HIV prevalence settings.
Study-specific aims are:
1. Sampling from RCCS-experienced and RCCS-naïve households, and using the MacCAT-CR, examine adolescent capacity to consent to biomedical research and correlates of that capacity. 1.a: Compare capacity to consent among early, middle, and late adolescents and their guardians. 1.b: Assess correlates of capacity, including actionable factors such as health literacy and education, and biomedical-related factors such as PrEP eligibility, use, awareness, beliefs, peer norms, and stigma.
2. Using a systematic qualitative analysis – guided by our conceptual framework for mapping age differences – examine processes of decision-making around biomedical prevention and biomedical research (e.g., stigma, understanding of biomedical prevention and research risks and benefits and constructs like randomization, privacy, safety, and autonomy) among guardians and early, middle, and late adolescents.
3. In partnership with US and Uganda researchers, and IRB members, construct a digital toolkit to support decision-making regarding key aspects of minor consent in low-resource settings. ICARE will provide guidance for ethical boards seeking to harmonize consent for adolescent healthcare and research to address disparities in research by age, and facilitate studies that prioritize adolescents to end the HIV epidemic.
Methods
ICARE uses mixed methods to describe adolescent capacity to consent to biomedical trials, such as HIV pre-exposure prophylaxis (PrEP) product trials. We examine age-related differences and identify actionable factors related to the capacity to consent to biomedical research.
We recruit equal groups of early, middle, and late adolescents and matched guardians from households that have participated in the open, longitudinal population-based Rakai Community Cohort Study (RCCS) and from households naïve to the RCCS (Total 438).

The study uses the MacCAT-CR to assess cognitive capacity to provide
simulated consent to an adolescent PrEP trial, modeled after HPTN 084 (Safety
& Efficacy of Long-Acting Cabotegravir for the Prevention of HIV), and
conduct additional qualitative interviews (n=25 dyads per age group) to
illuminate processes of guardian and youth decision-making. We will assess
whether age, gender, educational status, and literacy, as well as PrEP
eligibility, prior use, awareness, knowledge, stigma, medication beliefs, and
peer norms, are associated with cognitive capacity scores. This is a timely
moment to examine PrEP, an active area of global research with potential benefits
for youth.

Findings and Impact
Findings will be used to construct a digital toolkit for including adolescents in biomedical research for research ethics committees (RECs) and institutional review boards (IRBs). They will also contribute to addressing a major barrier to participation through an examination of a critical area in biomedical research ethics – the capacity of adolescents of different ages, levels of education, literacy, and need for prevention to comprehend elements of informed consent and, therefore, to self-consent. ICARE will advance the field by evaluating whether early and middle adolescents in Uganda demonstrate adult-level cognitive capacity to consent to biomedical HIV prevention research.
The PANGEA-HIV (Phylogenetics And Networks for Generalized Epidemics in Africa) consortium is a collaboration between scientists from the Rakai Health Sciences Program (Uganda), Africa Health Research Institute (South Africa), Johns Hopkins University (USA), Medical Research Council/Uganda Virus Research Institute (Uganda), Zambart Project (Zambia), London School of Hygiene and Tropical Medicine (UK), Imperial College London (UK), Partners in Prevention Project at the University of Washington (USA), Botswana Harvard AIDS Institute Partnership (Botswana/USA), University of Edinburgh (UK), and the University of Oxford (UK).
The overarching goal of the PANGEA consortium is to identify individual and population level factors that drive the epidemic using HIV-1 phylogenetic data, analyze the dynamics underlying the epidemic, and translate these findings into information that can be used to target HIV interventions more effectively. The RHSP is a major contributor to the PANGEA consortium through several samples collected within the ongoing, open, population-based Rakai Community Cohort study. To date, PANGEA has generated and analyzed over 40,000 deeply sequenced HIV genomes from eastern and southern Africa (Rakai, Uganda; MRC, Uganda; PopART, Zambia; BCPP, Botswana; and AHRI, South Africa), and revealed a lack of large HIV phylogenetic clusters suggesting that most new HIV diagnoses have occurred sporadically across several transmission chains within individual African communities. This suggests that HIV transmission in Africa remains broadly generalized, in contrast to European and American HIV epidemics which are concentrated in key populations and more work utilizing multiple population sampling strategies may reveal crucial targets for enhanced epidemic control amidst declining HIV incidence in sub-Saharan Africa.
REACH (Research Enterprise to advance a cure for HIV)
The REACH study is a NIH based Martin Delaney funded consortium that seeks to foster dynamic, multidisciplinary collaborations between basic, applied, and clinical researchers studying HIV persistence and developing potential curative strategies. The RHSP runs a HIV cure study cohort of 90 HIV positive individuals who are contributing to a greater understanding of HIV cure / viral persistence from an African perspective. Through this cohort (initially funded by NIAID), baseline estimations of reservoir size and differences have been described among Ugandan men and women compared to Americans. Interestingly, transient declines in replication competent viral reservoir size have been described following DTG rollout and further work is ongoing, including that based on onsite technology transfer of ddPCR platform technology (IPDA assay) to better understand underlying mechanisms of viral reservoir persistence, trends/evolution, and possible targeting towards eradication.
The INSTEP (Integrated Female Sexually Transmitted Infection Testing for HIV Epidemic Control through PrEP) study
The INSTEP study is a new study being rolled out at the RHSP. INSTEP is a randomized trial assessing whether access to integrated curable STI (cSTI) testing will improve PrEP use among women in Africa and seeks to provide compelling evidence on critical effectiveness, implementation, and modeled data to influence policy and programmatic decisions that will inform strategic delivery of high impact HIV prevention. STIs are a risk factor for HIV acquisition and are used as a self-screening tool prior to PrEP enrollment in Uganda but unfortunately, over 85-90% of STI episodes may be symptomless. STI laboratory diagnosis is costly and not widely available in Africa, and this implies that a significant number of persons with symptomless STIs, especially vulnerable females may not perceive themselves to be at risk/PrEP eligible. Our preliminary observational data suggests a high burden of undiagnosed cSTIs among African women at high risk for HIV and that adding cSTI diagnostic testing to existing PrEP eligibility screening efforts would nearly double the number of PrEP eligible women. Preliminary data also show women with cSTI symptoms are more likely to perceive themselves as being at high HIV risk, and that women diagnosed with cSTIs are more likely to use PrEP. Thus, INSTEP aims to individually randomize enrolled females to the standard of care self-risk screening tools for PrEP eligibility (with syndromic STI management) versus self-risk screening plus cSTI diagnostic testing for chlamydia, gonorrhea, trichomonas, and syphilis to increase PrEP use among cis-gender African women aged 15 to 39 years in the RCCS cohort.
Specific AIMS
1. Conduct an individually randomized effectiveness implementation trial of self-risk screening alone versus self-risk screening plus cSTI testing to increase PrEP use among African women at high HIV risk. ~4,500 HIV-negative women will be randomized 1:1. Primary outcomes will be PrEP uptake after screening and adherence and persistence at 6 months assessed through survey, clinical records, and drug level testing.
2. To perform a mixed-methods, implementation science evaluation of female cSTI testing for improving PrEP use for HIV prevention. We will use qualitative and quantitative methods to assess mechanisms, barriers, and facilitators to improving PrEP outcomes through cSTI testing and how this varies by cSTI pathogen, SRST outcomes, and demographic profiles.
3. To determine the most efficient, population-level female cSTI testing strategies to reduce HIV incidence in African settings. We will use data and results from Aims 1 and 2 to inform mathematical models which will evaluate different cSTI testing approaches to reduce HIV incidence at a population level by considering what cSTIs to screen for, in what health care settings, and at what cost thresholds.
Mental Health And Cognition in HIV Infection in Rakai Uganda extended Rakai Neurology Cohort Study (EXRNCS)
Background
Central
nervous system (CNS) complications in HIV infection persist despite effective
antiretroviral therapy (ART) and impact HIV care including ART adherence
particularly in resource-limited settings. Two of the most common, often
comorbid CNS complications in the current era are major depressive disorder (MDD) and
neurocognitive impairment (NCI).
Study goal: This study set to
evaluate the mechanisms of mental health disorders including MDD and NCI more
broadly with detailed evaluations and a novel methodology. The study focuses on
several key pathways with strong scientific premise for contributing to MDD and
NCI that could result in novel peripheral biological signatures of MDD, NCI, or
the combination of the two in the context of viral suppression: neuronal/axonal
injury, inflammatory, and novel exosome markers. The study also evaluates the
significance of viral compartmentalization on long-term MDD and
NCI.
Study procedures: We proposed further follow up, new assessments for additional mental health disorders, and laboratory investigations among PLWH on long-term ART to improve our understanding of the causal mechanisms of mental health disorders and NCI in PLWH, with primary focus on MDD and NCI. Data on anxiety and stress which are often comorbid with MDD, will also be collected,
The study will examine the role of plasma markers of neuronal injury and inflammatory markers from exosomes derived from brain but obtained in the blood, and their association with MDD and NCI which have not previously been examined in PLWH in SSA.
Study Design for the extended Rakai Neurology Cohort Study (exRNCS)
Participants. The study has enrolled 350 people living with HIV (PLWH). These have had a baseline visit and a follow-up visit at 24 months after enrollment. Controls: From the Rakai Community Cohort Study (RCCS), we also recruited 250 HIV-negative (HIV-neg) controls who were age, sex, and community-matched to the PLWH. The goal of recruiting HIV-neg controls was to obtain normative mental health disorder data, neuropsychological testing and blood and CSF control data. Archived blood and CSF specimens are also available from 400 HIV-neg controls from the Rakai Neurological Cohort Study (RNCS) to serve as additional HIV-neg control data for the proposed markers.
Exclusion Criteria: severe cognitive or psychiatric impairment precluding written consent, physical disability preventing travel to the RHSP clinic for study procedures, known CNS opportunistic infection (e.g., cryptococcal meningitis), or prior CNS disease (e.g., stroke).
Recruitment. During the Baseline and follow-up for PLWH and HIV-neg controls, individuals had first clinical assessment and optional lumbar puncture (LP). All participants will have a two-year follow-up 24 months after enrollment visit, with identical assessments including the optional LP.
Study procedures. The same battery of assessments are administered at both study visits for PLWH and HIV-neg controls. The complete testing visit required ~5 hours. Our battery was chosen to provide all of the necessary information to diagnose HAND with a NP test battery to determine NCI, functional status assessment to determine activities of daily living impairment, and neuromedical exams to evaluate for confounding conditions.
General Health. Participants are administered a structured questionnaire to record sociodemographic characteristics, health and health care utilization, ART adherence, alcohol use /abuse, smoking, sexual behaviors, HIV prevention behaviors, use of non-ART medications, and disability. Symptom reporting includes symptoms within the past month and past year to reduce recall bias. A general medical exam is also completed.
|
Uganda Neuropsychological Test Battery |
|
|
Test |
Domain Assessed |
|
International HIV Dementia Scale (IHDS) |
Verbal memory, motor & psychomotor speed |
|
Timed Gait |
Simple motor skills |
|
Grooved Pegboard–Dominant, Non-Dominant |
Psychomotor speed |
|
WHO/UCLA Auditory Verbal Learning Test |
Verbal memory |
|
Color Trails |
Attention/information processing; executive function |
|
Verbal Fluency (FAS) |
Verbal fluency and executive function |
|
Symbol Digit Modalities Test |
Psychomotor speed |
Neurological Evaluations. Evaluations include: 1) Neurological symptoms questionnaire; 2) Neurological exam; and 3) Uganda Neuro psychological Test Battery
MDD and other mental health assessments. All participants complete the Structured Clinical Interview for DSM-V Axis I Disorders (SCID-V) to assess current and lifetime mental health disorders as well as mental health questionnaires including: the Childhood Trauma Questionnaire, Patient Health Questionnaire (PHQ)-9, Generalized Anxiety Disorder Screener (GAD)-7, Center for Epidemiological Studies-Depression Scale (CES-D), PTSD Checklist-Civilian version (PCL-C), Perceived Stress Scale-10 (PSS-10), Beck Anxiety Inventory (BAI), the World Health Organization (WHO) Violence Against Women Questionnaire, sexual coercion questions from the Rakai Project, and domestic violence questions from the community HIV epidemiological research (CHER) survey-2 (adapted from the Conflicts Tactics Scale). These assessments will allow us to examine anxiety, PTSD, and alcohol abuse in addition to MDD.
Behavioral & Self-Report RDoC Assessments. Behavioral and self-report measures to assess the RDoC domains of declarative memory, cognitive control, and NVS are also assessed.
Empowering Our Communities: Health Education and Community Mobilisation (HECM)
The Health Education and Community Mobilisation (HECM) section serves as the vital link between the Rakai Health Sciences Program (RHSP) and the communities where research and program activities are carried out. With a primary focus on community engagement, the HECM section plays a pivotal role in fostering awareness, participation, and collaboration within these communities.
Core Functions
- Community Awareness: The HECM section is dedicated to raising awareness about RHSP research initiatives, as well as the various services and programs offered. Through targeted educational campaigns and outreach efforts, community members are informed about the importance of research participation and encouraged to actively engage in RHSP activities.
- Compliance and Participation: By fostering a sense of ownership and involvement, the HECM section aims to increase community compliance and participation in RHSP endeavours. Through community mobilisation efforts, individuals are encouraged to take an active role in their own health and well-being.
- Friendly Environment Creation: Creating a welcoming and supportive environment is paramount to the success of RHSP activities. The HECM section works to cultivate positive relationships and trust within communities, ensuring that research and program activities are conducted in a manner that is respectful and responsive to community needs.
Additional Activities
- Dissemination of Research Findings: The HECM section ensures that research findings are effectively communicated to the communities involved, fostering transparency and accountability.
- Preparation for Services: Communities are prepared and informed about the various services offered by RHSP, facilitating access and utilisation.
- Community Advisory Board (CAB) Collaboration: Working closely with the Community Advisory Board (CAB), the HECM section facilitates dialogue and feedback between research communities and RHSP, ensuring that research activities are conducted in a manner that is ethical, respectful, and beneficial to all parties involved.
The HECM section serves as a cornerstone of community engagement within RHSP-supported areas. By fostering awareness, participation, and collaboration, the section contributes to the success and impact of RHSP research and program activities, ultimately improving health outcomes and well-being within the community.
Join us in our mission to advance health research and improve public health outcomes globally.
Collaborate for Health, Innovate for Impact.